Fixing the looming healthcare crisis with technology

HEALTHCARE IS UNDER PRESSURE FROM SEVERAL DIRECTIONS. CORILUS IS CONNECTING THE STAKEHOLDERS IN THE SYSTEM TO RADICALLY STREAMLINE PROCESSES.
Increasingly, elderly care is becoming a multidisciplinary task requiring coordination between rest and nursing homes, general practitioners, physiotherapists, nurses and pharmacies. As institutional care is extending towards home-based care, the need for efficient coordination among the various actors in the system will only increase. Corilus, a leading ICT-provider for healthcare professionals and rest homes, is aligning itself to eHealth with open standard solutions for managing processes that cross organisational boundaries.
Healthcare under pressure
We’re acutely aware of the fact that the healthcare sector is under pressure; it needs to adapt to a number of clear trends and challenges. Firstly, demand for healthcare services is gradually increasing and will continue to increase in the coming years. Partly this is due to the ageing of our population. Older people require more care and are more likely to suffer from chronic illnesses.
Even among younger people, however, the prevalence of chronic illnesses such as obesity and diabetes is increasing. In parallel to these trends healthcare is becoming increasingly high tech—which requires important investments. And the regulator is adding pressure too by raising the bar on quality control and the traceability of medication. These trends all combine to drive healthcare costs upward—just at a time when governments are trying hard to reduce spending. And just to top it all off, there is an increasing shortage of healthcare workers, especially nurses. The sector is under pressure to expand, but it is restricted in doing so due to a shortage of money and people. That’s why ICT is destined to play such an important role in healthcare by saving time and creating more efficiency.
With the Healthcare sector under pressure, it needs to adapt to a number of changes and technological developments to overcome the challenges. The cost from local GP’s to Glasgow orthodontist, hospital staffs to A&E departments are significantly increasing meaning these services will become more expensive as more nurses, doctors and dentists are hired to cope. With such a high demand technological innovation offers our healthcare system a solution to cope with the current crisis.
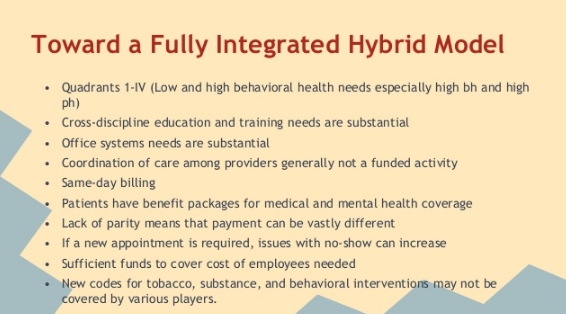
Toward a hybrid model of care
It is interesting to see how these trends play out in one of our core markets, Rest and Nursing Homes. At present elderly care is concentrated at the institutional level, at the rest homes. However, in the years and decades ahead we cannot meet rising demand simply by building more rest homes. At Corilus we believe that the system will move towards a more hybrid model where all actors in the elderly care system—GPs, rest homes, nurses, pharmacies, physiotherapists, etc—will coordinate their work around patients who remain at home.
Today rest homes already have a support function to home care, but this will become more intense in the years ahead. They’ll increasingly need to offer people day-care services or short-stay services. Also, we predict that rest homes will play a central role in the coordination and alignment of home care.
A Patient Empowerment Activist

In 2007 Dave deBronkart was diagnosed with late stage kidney cancer. After a miraculous recovery, he decided to turn his expertise to helping empower patients in an effort to transform the healthcare field. Now an advocate, activist and proud e-patient, deBronkart shares his ideas for taking advantage of the information explosion to create a new, improved way for patients and the medical field to interact.
What makes an “e-patient”
After my diagnosis, I was given 24 weeks to live. That tends to focus the mind. When I beat the disease, I faced life with a whole new view. A year later, my physician enrolled me in an e-patient study group.
E-patient means “empowered, engaged, equipped, enabled” it means people taking charge of their own medical care and not depending on the system. The founders of this idea saw that with the internet patients would have access to things formerly only available to physicians. Now patients could have better information, connections with other cases, and so on.
When it was first developed, the “e” was popular for everything online. Today, being online does not make you an e-patient. Many people are online and remain very much not empowered.
The main “e” today is being an engaged patient instead of a passive recipient. You can be an engaged patient with or without the internet. If patients are highly activate partners in healthcare, that just brings an enormous new resource to the transaction, and it’s a resource that has been highly missing.
Patient empowerment means patient engagement
There are lots of definitions of patient empowerment. For many people, “patient empowerment” is shorthand for “watch out, medical errors happen all the time and you or your family may get harmed. So be aware.”
However, I’m a child of the ’60s. I watched the civil rights movement and the women’s liberation movement. I watched as people became empowered. To me empowerment means people being able to say what they want. Empowerment means people speaking up for themselves instead of feeling “no, I can’t say that.”
Many people get into patient empowerment after medical disasters. I came at it after being the recipient of a miracle cure. My diagnosis, treatment and hospital care were all superb. But as I studied healthcare, I began realizing there were massive inefficiencies in this field. Even where healthcare is efficient, it’s not accomplishing what it could. There’s this mythology built up around the medical field, and that has to change.
How patients are changing healthcare
Like the medicines that ended up saving my life, there are treatments that are not well understood by the medical community but are understood by the patient community. It raises the question: how could it possibly be that scientifically accurate information is more readily available among patients than among many doctors?
Twenty years ago this would not be true. At best, through dumb luck you might bump into somebody at a diner with valuable information that’s not available from most doctors. But today it’s very common.
For example, when interleukin, the medicine that saved my life, was first approved, it worked on seven percent of patients and four percent died. But by the time I underwent treatment four years ago, it was up to 20 percent of patients working, and they haven’t lost a patient in nine years. Things have drastically improved.
But your average oncologist doesn’t see a kidney cancer patient that often, they don’t know this.
Doctors are under increasing pressure to see more and more patients; there’s an explosion in the number of diagnoses possible. There’s also an explosion in journal articles. The doctors are simply overwhelmed.
In contrast to that, my kidney cancer patient community has one area of focus: we can go deep and wide. We can examine these topics in a detailed way that most physicians simply don’t have the ability to do by themselves.
This is a cultural problem, and there’s some pretty aggressive pushback from doctors superstitiously disbelieving how overwhelmed their profession has become. They have this belief that of course their support systems are keeping them up to date on everything they need to know. But it can’t. It’s not their fault; it’s a product of the information explosion.
The time it takes to go through the journal process — from getting the information to it landing on a doctor’s desk — is two to five years. If you have an estimated survival time of 24 weeks and there may be life-saving information out there that’s still working its way through that pipeline, this is a problem.
The problems with the established medical information “pipeline”
It’s true that valuable information can exist outside the medical pipeline. It’s true that people, without medical training, can hunt and find that information. It also explains why this whole thing has blindsided the establishment. They simply were not aware this was happening.
More enlightened doctors, especially those coming out of medical school now, get that this change has occurred. They’re beyond simply using e-mail; they’d rather IM with their patients.
But the assumption in the establishment is that it will upgrade itself. They cannot do this because they have out of date information and the old methods simply can’t keep up. If you’re in a medical crisis in this environment, it’s like stepping into traffic based on information that’s years old.
Think about this: your mother, your uncle, your kid is in a medical crisis. You want to save them and this is about as fundamental a need as it gets. So there is economic value in higher quality information, and it’s not coming from most hospitals.
Adapting patients — and doctors — to the new reality
A major goal is to get people adapted to the new reality. In some cases it clears up immediately. In others it requires transforming the culture, getting over people’s beliefs.
It turns out there are a certain percentage of people in the medical field — at least in America, but doubtlessly around the world as well — who are simply assholes. They have a god complex, they don’t want to change, and some of them get belligerent.
For example, my sister had a severe case of stomach pain. In her particular doctor’s office, it was the receptionist who was empowered to filter out who she thought should see the doctor. She told my sister that there was just a stomach flu going around. Finally she forced her way back in there where she saw a physician’s assistant who put her on an ambulance and rushed her to the emergency room. She had a major gallbladder problem; it was infected and hemorrhaging. She was hospitalized for two days.
In this case, her primary care physician was no longer taking her phone calls, and she would have died if she had followed their advice. But she knew to speak up for herself. That has nothing to do with better access to information on the internet; that’s patient empowerment of a different sort, and it’s just as vital.
There’s awakening people to this new reality — that they have information at their fingertips that simply wasn’t there two decades ago — but just as importantly, there’s a need to change the culture so they’re the ones empowered.
TED, the iPad and the quest for participatory healthcare
How do you encourage a large university hospital to make the transition to participatory healthcare? “Develop a Swiss army knife”. Lucien Engelen and his team at the Radboud Reshape & Innovation Center are addressing the problem in a multi-pronged but highly pragmatic manner. Firstly, they’re getting healthcare workers to talk about the issues. Not by handing out flyers, but by organizing fun Pecha Kucha sessions and what could be Europe’s largest TEDx event yet, focused exclusively on the future of healthcare. Secondly, they’re facilitating real change in the hospital’s work processes. Not by launching a major ‘change’ project but by experimenting with consumer technology—such as the iPad and Skype—that lowers the threshold for patient participation.
Can you tell us a little about the Radboud REshape & Innovation Center?
The Radboud REshape Center was set up by the end of 2010 when the Executive Board of the Radboud University Nijmegen Medical Centre as part of the adopted strategy that we need to transition toward participatory healthcare. This was a pretty fundamental decision, as a result of intense discussions I had with the board, for the hospital because it touches on the core of what we are,. It acknowledges that there probably is nothing as paternalistic as a hospital and that a total mental shift will be required if we are to succeed. At base it means that we need to start informing patients in such a way that they are able to make decisions—together with the physician—about their treatment.
Are people ready for that responsibility?
Not everybody but you have to look at this from a long-term perspective. Innovations typically take about 7 years before they lead to real societal change, al least in healthcare. It is true that the generation requiring care now does not need or want computers, but the generation coming in was brought up with computers. Even today’s diabetes generation is young enough to have been brought up with computers. It’s difficult to say how exactly this will evolve but attitudes and expectations are definitely changing. For example, my son looked at me as if I was crazy when I tossed away a phone book delivered by mail, when I told him what we used to use it for. They think differently, not only about communication but also about work processes and power relationships.
I’m convinced that the patient-doctor relationship and the role of the doctor in particular, are changing significantly. The doctor’s role will evolve to a more consultative and coaching role. In the 10 minutes they have with a patient they will have to focus on the right questions, helping patients make sense of the information and come to decisions. The problem is that patients only process about 20% of what is said during a consultation. That’s why technology can really make a difference to improve communication. Although I do want to make clear that Health 2.0 is not primarily about technology; it is about attitudes, roles and work processes.
Tell us about some of the innovation projects initiated by REshape
I like to think of our Reshape-programme as a Swiss army knife; it’s multipronged initiative. We do research, we organize events and conferences, give lectures and workshops and we initiate innovative projects. There is no silver bullet to transforming healthcare. We have to work at different levels. For example, the conference call system I’m using now to talk to you is an open platform (Skype). We’ve made it available for multidisciplinary consults but we specifically went for an open system so that patients and their relatives can join in too. The idea is to place the patient in a much more central position. So we’ve adapted this “consumer technology” to help patients to enter our newly developed video-conferencing system FaceTalk. Once they are in, our secure system takes over. So we use standard technology to lower thresholds and broaden the use.
We’re handing iPads to patients to show short films about what they can expect in their treatment. And for young adult cancer patients we’ve created a community to address specific challenges around identity, sexuality, careers, etc—concerns that are very specific to the 18-35 age group. With regard to the technology it is important to avoid creating islands. That’s why we use proven consumer technologies and simply add extra elements or combine techniques to simply create a new service for the care environment. Obviously you can build huge proprietary systems but there is no point in that.
To spread the message and stimulate debate on Health 2.0 we’re using events—again using proven concepts. Pecha Kucha (a popular event format where presenters show 20 slides, in 20 seconds each) is a great technique to liven up presentations and to ban keynotes with 120 slides or more. We started by bringing in external people to present material but now we’re seeing some of the doctors take up the challenge to present their experiences. It is a great way to stimulate dialogue, to look at your message, not only content wise but into design as well. And in April we have our first major conference, TEDxMaastricht. This is going to be one of the largest TEDx conferences in Europe to date—900 seats—and it will be dedicated entirely to the future of healthcare. Live streams in HD will be broadcasted to simulcast locations like Darwin Australia, Stockholm Sweden and many other places taking the amount of real-time visitors up to 10.000.
What is the higher goal of your organization? Is there really anything wrong with healthcare today?
Absolutely, there is something very wrong with healthcare. At present it is mainly one-directional traffic. Doctors say that they talk to patients; perhaps so, but there isn’t real negotiation with the patient. For a doctor, the patient too often is simply a disease that generates data on which they base their medical decisions. There is no real co-decision. Our mission is to inspire our colleagues to take a different approach to healthcare. And we’re doing that in a piecemeal fashion; via small steps and proven methods we gradually want to change the way healthcare is done, but sometimes we have to use way’s never explored until now. In a way, we’re trying to seduce our colleagues to work differently. We want to offer tools and services that really appeal to people. It is the little things that count here. That’s why we’re using the iPad as an enabler—people want to use it. FaceTalk is another example. Technology can’t be a barrier; it needs to be an enabler, something that will seduce people into behaving differently. But again, Health 2.0 is not simply about technology. In fact, you can apply Health 2.0 without technology. Ultimately it is about co-decision.
Healthcare professions tend to think that they know what the patient needs. That is not (always) the case. We see this time and time again. The whole sector is evolving with only one group in mind—the people who need care now, but it should also be preparing for the next generation coming in.
Why now? If Health 2.0 isn’t about technology, why is it making inroads now?
I think it has to do with the internet and the wider cultural shift that it is driving. This isn’t only about healthcare—you can see similar trends everywhere. It is about information access, or rather, the democratization of information. And it is about the increasing power of social networks.
For physicians this can be difficult to adapt to, especially because patients differ in their approach to seeking out and using information. Some are proactive researchers who confront their doctor with mountains of data and information. But there are others who are silently ‘testing’ their doctor’s expertise. It is so difficult to integrate this into the education of doctors. But technology is opening up opportunities here.
It is really important that we prepare ourselves now, so that we can be ready in a few years to cope with the impending changes, not only in patient expectations but also the problem of staff shortages, increasing healthcare costs and exponential healthcare demands.
Are you optimistic about change in the healthcare sector?
I’m an optimist at core, but also a realist. It will take years. The danger is that we keep talking about change but nothing really happens. In the healthcare sector we’re not very good at making changes, at making decisions—we talk too much. But that is no excuse because it is an ethical decision. It is unethical to delay; we need to get cracking on this. That’s why with our innovation center we concentrate on short 30-day projects to rapidly test things in a real world setting. And yes, we fail sometimes as well, but we will know within 30 days and hence can quickly cut our losses. This is in contrast to most e-health projects that fail because they are far too large and complex. And they tend to have very few generic elements in them. All our projects rely on generic components—on proven consumer technology—so that ultimately we can involve the patients in these projects, also from home. It is so important that these services are light, easy and accessible.
Obviously I don’t want to argue that we should kill all the large e-health projects but I do feel that there should be more programmes for supporting small projects, because I think it will ultimately be the small projects that
How innovation could transform health care
Innovation is a wonderful phenomenon. It leads to all sorts of astonishing products and services like the internet and the tablet PC. As big an impact these innovations have on our lives, it is in health care that innovation is of existential importance. To be blunt, innovation in health care matters because most of us will have to face a miserable disease at some point in our lives; and all of us will have to face death. If we continue to innovate, then one day in the future people may not need to undergo the distress of cancer, heart disease or Alzheimer’s. Perhaps we even await a future where we transcend the limitations of our physical bodies—as imagined by science fiction authors like Peter F Hamilton and predicted by futurists such as Ray Kurzweil. Today, however, we have to make do with our present health care system—and its challenges and limitations.
Life is short
The challenges are diverse. The most fundamental limitation is the fact that most of us continue to suffer from a number of persistently incurable diseases. Even in the European region, where life expectancy is relatively high, the healthy life expectancy is only 67 years (1). That is just too short given the number of things that most of us would like to do in our lives.
Inequality
Perhaps most deplorable, however, is the gaping inequality in the world when it comes to health and health care. According to the 2010 statistics of the World Health Organisation, life expectancy in the European region averages 75 years; in the African region it is 53 years (and healthy life expectancy is only 45). In Africa the probability that a child will die under the age of 5 is 142 per 1000 live births; in Europe that number is 14 per 1000 live births. In Africa there are 2 doctors per 10,000 population; in Europe that figure is 33. Notwithstanding the wonders of the digital era, when it comes to health and health care much of the world lives in medieval circumstances.
Inefficiencies in the developed world
In much of the developed world we tend to celebrate the excellence of our health care systems. Given the progress in recent years (life expectancy in EU countries has increased by six years since 1980) and the inequality in the world there is some justification for such celebration, but more likely it has to do with our psychology (don’t bite the hand that feeds you). The facts are that health care in the developed world can be managed better. The OECD has calculated, for example, that life expectancy could be raised by more than two years in the OECD area if all countries were to become as efficient as the best performers (2). The OECD is specifically talking about ‘efficiency’ here; according to the same OECD study, simply throwing more money at health care is unlikely to have much impact on health outcomes in the OECD area.
Looming crisis
Efficiency will also be important to deal with the looming budgeting and staffing crisis in most OECD countries. Health care costs are increasing rapidly, mainly due to the rising costs of drug development and medical technology. And in Europe the situation is exacerbated by the ageing population and increasing prevalence of chronic illness. In 2008, EU countries spent, on average, 8.3% of their GDP on health, compared to 7.3% in 1998 (3). Budgets often have been rising faster than GDP. Clearly this is an unsustainable situation for most EU countries, especially given the need to reduce budget deficits following the financial crisis. Not only is the ageing population driving demand for health care, it is also leading to shortages of nurses and other health care workers in many European countries. And this while nurses are set to play an increasingly important role in a health care system that will be overwhelmed by the elderly and chronically ill.
What can be done to address the above outlined challenges? Fortunately, there are at least three broad innovation trends that could ensure continued progress in the state of our health.
Post-genome paradigm
Firstly, medical science appears to be standing at the cusp of what some call a post-genome paradigm shift. Recent advances in genetics and genomics are ushering in the personalization of medicine where treatments are customized to the genetic profile of each individual. It is also enabling us, as patients, to gain insight into our individual risk factors for certain types of diseases—via DNA genotyping services like 23andme—and make appropriate lifestyle changes to minimize risk. Other exciting developments are the recent inductions of pluripotent stem cells (transforming mature body cells into stem cells that, in theory, are able to produce any body part) (4) and the ‘programming’ of cell DNA by researchers at the J Craig Venter Institute. It is these types of developments and what in effect is the increasing digitization of biology that suggests that one day we may be able to program life (“wetware”) much akin to the way we program software today. In a parallel to what has happened in the software development business, the biotech sector is now also seeing an increasing number of open source initiatives such as the Pink Army Cooperative (focused on breast cancer treatments using synthetic biology) and Bio Bricks (a registry of standardized DNA sequences for use in synthetic biology).
Reverse engineering health care
A second major trend is the economic rise of India and the way it is spurring innovation in low-cost health care services and medical technology. Emerging regions with a strong entrepreneurial drive have one great advantage over developed regions when it comes to innovation: they’re less encumbered by legacy infrastructure and vested interests. It is probable, therefore, that much of the innovation in telemedicine, medical technology and new health care models will come from countries like India. Entrepreneurs are able to experiment with new models in part because there is unmet demand for health care services and partly because they’re less likely to provoke the types of interests groups (hospital groupings, doctor associations, etc) that control health care in Europe.
Examples abound of entrepreneurs experimenting with new business models for the delivery of health care. LifeSpring Hospital is an Indian network of small (20-25 bed) maternity hospitals that is able to deliver world-class maternity care at remarkably low cost. Mothers pay 4000 rupees (€65) for a normal delivery. LifeSpring’s business model works because its operation is highly standardized and process-driven. This increases efficiency but also makes the model easy to replicate across India and possibly worldwide. At the total other end of the scale, Dr. Devi Shetty is trying to build huge “health cities” across India that are specialized in complex disciplines such as cardiology, oncology and organ transplant. Again, it is via process innovation, not product innovation, that health care is becoming more accessible to India’s population. Dr. Shetty’s 1000-bed cardiology hospital in Bangalore, for example, is able to price cardiac surgeries at less than $3,000 and his goal is to reduce it further. The Narayana Hrudayalaya group is also making active use of telemedicine to extend its reach. For example, it has treated nearly 70,000 heart patients via its Tele-Cardiology program (using satellite technology).
This level of ambition and total willingness to do things differently if it saves costs and improves accessibility is difficult to imagine in the European context. These are just two examples but there are numerous cases of innovation in telemedicine (e.g. ReMeDi remote diagnostics kits by Neurosynaptic), low-cost medical devices (e.g. Forus Health) and low-cost health care delivery (e.g. Aravind Eye Hospitals).
eHealth
The third key trend that is making a difference in health care is the use of IT and the impact of the internet more generally, especially in the developed world (and the US more specifically). Over the last two decades IT has gradually been making a bigger impact on the way health care is organized. In Europe the first wave of automation was focused mainly on administrative and logistical processes at hospitals, although even today there is still opportunity for greater efficiencies. As it stands, the market for hospital IT systems is still relatively immature and fragmented, mainly because the regulatory environments and financing models differ substantially from country to country. As a result, many hospitals have developed their own systems or the market is dominated by local IT providers.
In a second wave, IT entered the clinical domain via the introduction of digital imaging technology and electronic medical records. Simultaneously, national governments started developing eHealth strategies to improve coordination across the entire health care system. A recent study by the European Commission (5) concludes that substantial progress has been made in that regard, with most EU member states having in place policy initiatives for Electronic Health Records (a summary health record that would make basic patient health data available to any health care professional whenever and wherever as needed), Electronic Prescriptions (to reduce the paper trail and improve safety by, for example, relying on systems that alert doctors and pharmacists about potential contra-indications or fraud), and Telemedicine (to connect rural patients to health care professionals and to facilitate home-based care for patients with chronic conditions). However, the same report concludes that most member states radically underestimated the implementation challenges inherent to eHealth strategies.
It has turned out to be tremendously time-consuming to reach agreement on eHealth strategies among the core stakeholders within the health care system. This delays implementation and creates problems during implementation if some stakeholders actively resist new methods. As a result, the actual implementation of eHealth strategies has, to date, been less successful in Europe. For example, while every EU member state has an EHR policy initiative, only 7 EU member states are routinely using EHRs. Some member states have also changed tactics, replacing top-down centralist approaches (imposing new standards and tools on health care providers) with a more decentralist, bottoms-up approach (creating incentives and setting standards but letting the market take the lead in implementing systems).
The power of data unleashed
IT is also gradually being used by health care providers in Europe to improve clinical processes and support clinical decisions. As illustrated by the Indian cases studies, this could have a tremendous impact on efficiency. Moreover, it could also significantly improve the quality and outcomes of health care. One of the key benefits of eHealth will be the tremendous amount of data that is gathered automatically via Electronic Records and Decision Support Tools. The countries that have made most progress implementing eHealth technologies (such as Israel and the Scandinavian countries) are now beginning to put their data to use to improve health care.
Health 2.0
While eHealth may be suffering somewhat from the trough of disillusionment, a new trend is emerging that is rapidly climbing the first ascent of the hype cycle: Health 2.0. In the period that health care providers and policy makers argued about how to manage the patient data they controlled, patients have been discovering the liberating effects of the internet and social networks. Over the last two decades patients have gained, via the internet, near unlimited access to the world’s stock of medical information. A motivated ePatient (using ePatient Dave deBronkart’s terminology, referring to engaged, empowered, equipped and enabled patients) can, with some effort, become a better expert on his or her disease than the attending physician. And in recent years, patients have begun forming social networks for sharing medical information. Via online platforms like CureTogether and PatientsLikeMe, people are able to compare their symptoms with each other and share advice about treatments and medical providers. Much of this information sharing is happening in a structured way enabling data mining and research. CureTogether, for example, recently reported a link between infertility and asthma (members with infertility are 40% more likely to report asthma). Patients are being empowered with highly focused, relevant information and medical science gains too because so much additional data is becoming available. All this is placing significant pressure on health care providers to adapt to these new realities by improving patient communication and moving to a more participatory style of health care provision. While many health care providers are still arguing about eHealth strategies and implementing heavy-duty IT systems, the institutions that ‘get it’, such as Radboud University Nijmegen Medical Centre in the Netherlands (see our interview with Lucien Engelen), are taking a closer look at consumer technologies and open internet platforms that lower the threshold for patient participation.
Opportunities
So what does all this mean for innovative entrepreneurs? Where are the opportunities? Based on this summary of the key innovation trends in health care, the main opportunities are in more process-driven health care delivery business models, as is experimented with in India; in telemedicine and low cost medical devices (especially diagnostic devices), to extend the reach and accessibility of health care; in data analytics tools and services (e.g. see interview with Candace Toner of Biomatters), to tackle the flood of data coming from biotech on the one hand, and eHealth and Health 2.0 platforms on the other hand.
Helping hands – the vision of a complete health care eco system

Ergonomidesign is a design consultancy that has historically focused on designing devices that make life easier for people with disabilities. Their video “Helping Hands” portrays a future scenario for a health care system where every person will have instant access to their own biometric data, and where the process of getting diagnoses and treatments is remarkably more convenient than the conventional way. The CEO of Ergonomidesign, Krister Torssell, talks about their vision on health care, and the urge to modernise an ancient health care system.
The foundation for Ergonomidesign has always been the perspective of other humans. When the company started in 1969, we mainly focused on people with disabilities and different handicaps, and how to make life easier for them. We tried to make service conditions better and create tools that would allow disabled people to work as if they weren’t. We learned a lot in this process, and moving on to Life Science was a natural step.
Our goal is to increase the life quality for humans, and to use user-driven innovation and new technology to do so. Every day at the office, people share their visions and new ideas, and we discuss possibilities and scenarios for the future.
Channelling the ideas into a video
As we were preparing for the Medica Fair 2009, we wanted to gather all those ideas and visions into one scenario that would showcase what we want to tell the world, and what possibilities actually lie in today’s technology. That is how the idea of the video about the future of health, “Helping Hands”, was born.
Future health care through the lives of Bernard and Hannah
In the video, we follow two people using the future integrated health care services. “Bernard” is diagnosed with Coronary Arterial Disease (CAD), and is dependent on a healthy lifestyle and control over his own health. He carries a tiny elliptical CAD device with a customised software application, through which he can make sure the levels in his body are under control, and therefore control his disease. Bernard can access the information at all times thanks to advanced smart surfaces with multi-touch technology (e.g. phones and tables).
“Hannah” uses a General Health service that helps her keep track of her basic biometric data, like pulse, oxygen levels, tidal breath and blood pressure. When she meets Bernard, they log into their profiles and compare their data on a smart surface. Hannah realises that she has very similar biometric data to Bernard in the initial stages of his disease. Through this early discovery, Hannah can get professional help quickly and therefore has a better starting position for treatment and keeping the disease under control.
Rapidly developing technology
The video is a way of showing what can be done and how we as patients would benefit from using technology as we are used to in other areas, such as managing our economy. Thereby we will hopefully accelerate the development of better devices and most importantly – turning the integration of the different systems and devices into a working eco system.
“Helping Hands” displays a future scenario, but the development in other areas suggest that we soon will have the technology we need to make it come true. We see that different types of touch screens for different devices develop fast, on everything from phones to tablets. With the new types of sensor technology, it will be possible to measure blood levels and other biometric data, or use a dinner table as an integrated smart surface. The possibility of reaching information anywhere is also quickly developing as the number of applications for technical devices grows.
What we are doing in the video is merely applying technology that is more developed in other consumer products and services to a different scenario.
The crucial part – merging functions into a working eco system
A bigger challenge is how to merge all the different components together. It is an area where everything moves much slower. Another big question is what kind of organisation will actually build this system. The solutions will probably be different in different countries.
We have shown our vision of the future, and it is a realistic scenario. We know that many companies are already developing the different components in our future eco-system. Now it’s up to the health care industry to develop a sustainable system that is developed with a premier focus on the patient.
Why the current health care system needs to improve
There is so much room for improvement in today’s health care. Many people are frustrated by the slowness of the process we have to go through to even meet with a doctor. There are so many mechanic arrangements that don’t really have any value; it can take weeks or even months from the first contact with a health care provider to the diagnosis. With the new eco system, everything will be much more effective. The doctor will already be able to have your biometric data analysed when you get there. This way of working will not only make the process more effective, but also create time for the important human meeting. Also, all different caregivers will be integrated into one care-chain, increasing the doctor’s overall control of the patient.
Using technology instead of standing next to it
In today’s system, there is such a huge discrepancy between the health care system and the Internet. Anyone can search for information on the Internet, and even diagnose herself, often incorrectly. Many people do this because of the frustration of the slow health care system.
These problems must be solved and the industry must develop in line with the patients. It is surprising that things are moving so slow in an industry where there is an urgent need for improvement.
As a design company, we are sometimes looked upon as only caring about what looks pretty. With this concept, we wanted to show how design can develop life-changing ideas. Now, we just look forward to the ideas turning into reality.
IT is enabling evidence-based medicine
UZ BRUSSEL’S CLINICAL WORKSTATION STREAMLINES INFORMATION FLOWS AND ENABLES EVIDENCE-BASED MEDICINE
To streamline the massive information and clinical processes in UZ Brussel, the university hospital has developed a Clinical Workstation. Physicians and nurses use this system for almost all their activities, and it gives them a complete picture of the patient’s medical history. The Clinical Workstation even integrates clinical decision support systems, which help doctors to practice evidence-based medicine.
Since 2000, UZ Brussel is extensively using an in-house developed Clinical Workstation (CWS) to streamline the massive information and clinical processes in the university hospital. Rudi Van de Velde, CIO of the hospital, explains that this system is able to offer its users (550 physicians and 1400 nurses) a holistic view of their work: “With this clinical workstation, our users have access to all patient and hospital related information within one system using a consistent user interface, which minimises training and optimises the work experience.”
Physicians use the CWS for almost all their activities, including order entry, scheduling (radiology, pathology, surgical and other activities), reporting, medication and admission. Physicians also have a complete picture of the patient’s medical history at their fingertips: “We seamlessly integrate hospital applications, re-use many software components, and effectively manage change more efficiently. On a daily basis, physicians and nurses access patient records 25,000 times, schedule 4,000 appointments, capture more than 5,000 medical reports and process over 9,500 medical orders. Ninety percent of these interactions are completed in less than one second.”
Choosing to be Difficult
E-TRINITY, A LEADING HEALTHCARE SYSTEM INTEGRATOR, RELIES ON A UNIQUE METHODOLOGY TO DRIVE CHANGE IN THE HEALTHCARE SECTOR
e-trinity is purposefully changing the way healthcare is doing business. Its founder is attracted to the healthcare field because of its inherent difficulty on one hand and the potential and vital efficiency improvement of healthcare delivery on the other hand. This magnetic appeal of detecting improvement and defining solutions keeps Jeroen Van Maercke and his company e-trinity on the forefront of the healthcare evolution. Jeroen weighs in on why he’s drawn to this particular challenge and his hopes for the industry.
Facing the future
Healthcare isn’t sustainable. It is a failed state about to collapse. Healthcare delivery organizations are facing a huge challenge. They face a rapidly increasing demand due to the aging demographic. Meanwhile, both the evolution of healthcare and treatment possibilities are progressing vastly. Since the emergence of social networks and healthcare communities, the patient has been claiming a more active role in his healthcare and wellbeing. This in turn places pressure on the various healthcare organizations to redefine their mission and position in society. Last but not least, the increased financial stress on healthcare budgets forces healthcare organizations to optimize their processes and collaborate with others to limit and/or share their investments.
Gaining the necessary perspectives
I’ve always worked in healthcare, starting over 10 years ago with Quadrat in 1997. Industry has only one motivation – margin for profit – with a single leader responsible. It was here I climbed the corporate ladder until I worked on the global introduction and training of a software program. The years of traveling took its toll and in 2003 I opted for a job with the University Hospital Antwerp.
Instead of working for hospitals, I was in one. I soon learned that a healthcare organization is different from an industry organization. There is not a single leader in a hospital that can make decisions and be held solely responsible for them. Revenue in hospitals is generated by (often-independent) doctors utilizing and paying for the hospitals facilities. In many cases, the lack of clear responsibility resulted in conflicts of interest, power struggles on simple matters, and delayed business decisions. It was a frustrating experience that so few decisions were made and a limited amount could be accomplished.
A patient-driven approach to generating healthcare data
A SOCIAL NETWORK FOR CHRONICALLY ILL PEOPLE IS GENERATING A WEALTH OF HEALTHCARE DATA
While much of the debate about improving the United States’ healthcare system — one of the world’s largest — has centered around companies and government figures, the social networking website Patients Like Me has tried to approach the complex and often vexing issue by putting more information in the hands of individual patients, and inviting them to share. Co-founder Ben Heywood, currently the President and Director of Patients Like Me, believes a reassessment of privacy and better use of data is necessary to take healthcare into the 21st century.
A family tragedy led to the founding of Patients Like Me
Unfortunately my brother got diagnosed with Lou Gehrig’s disease back in 1999, so my family got really involved in ALS research. So my brother, Jeff Kohl and I decided to start Patients Like Me out of the experience of caring for our brother, researching ALS and talking to other patients about what they were going through. We found that there was a real dearth of information, for everyone, about what happened to “patients like me;” outcomes, symptoms, treatments that patients were taking. We saw there was really no good way of finding and sharing that information. Seeing that need, we started a registry on ALS in 2004, launched the first site in 2006 and have been growing ever since.
One of the core beliefs of Patients Like Me is that “information can change the course of a disease.”
It’s all about getting the right treatment for the right patient. In the healthcare industry as a whole, there just isn’t data that allows one to do that; it’s just not part of the system. Part of what the communities we create on our site do is help share that information. Our data sets have quickly become some of the largest in the world. We had a researcher on fibro myalgia talk to our community about eight months after our launch and he said “you have the richest data set on fibro myalgia anywhere in the world.”
How data can help solve the healthcare system’s problems
These data sets allow you to begin modeling a disease, so you can really understand what happens to an individual patient. That way, when something new comes on the market — a new drug, a new product, a biomarker, etc. — you can rapidly understand whether or not it works, and for which patients. One of the big problems with healthcare is that we don’t measure in the right ways. If you think about what you do in business or in your everyday life, one of the first steps is measurement. To measure is to know. When healthcare does measure lots of stuff, it doesn’t measure what’s ultimately most important: the patient’s quality of life. In the realm that we deal most in — chronic conditions — there’s no measurement over time. The data our patients provide becomes an incredible source for measuring value, then you can spend healthcare dollars where they’re most valuable instead of just spending healthcare dollars, which is what happens now. Patients can browse and use the data to better understand their own — or others’ — conditions, and the data can prove useful to other parts of the healthcare system as well.
Sometimes being able to see other patients’ experiences acts almost like a kind of intervention; 20 percent of people in our mood disorders community, for example, actually report needing less care because of being a member of patients like me. That lowers healthcare dollars.
Primarily we’re also partnering with pharmaceutical companies who really want to understand — from a clinical standpoint and a market standpoint — how patients are experiencing their disease and how they perceive and utilize their products and services. This allows the company to improve their product; it’s a way of partnering companies and patients together around the data that’s being shared in the community.
People are used to being very private about their healthcare situation, and there are laws that back that up, making access to healthcare information stricter than almost any other sort of record. But there are issues with that mentality.
Every day, millions and millions of dollars are spent, trying treatments, whether they’re old and true methods or newer, more experimental ones. But often we don’t learn from all that trial-and-error, because this data isn’t collected. Even when it is collected, this important information is usually kept siloed in hospitals or universities. The reality is, there’s tremendous value in sharing that information.
All of these privacy protections that have been put in place are actually, as a society, reducing our ability to further research disease states, reduce healthcare costs, and have real conversations about the tradeoffs of treatments for different diseases.
The beauty behind our openness philosophy is that people learn that when they start sharing what happens to “patients like me” they can learn about their own healthcare and help the whole society.
Social networking improves patients’ wellbeing
Some of these diseases are very isolating, and with that isolation comes depression, which only worsens the condition. Having a social connection is healing in and of itself. Knowing that sharing this information is helping yourself and others is another way it improves a patient’s quality of life.
Also, we hear all the time from patients in our multiple sclerosis community, for example, that “the rest of the people in my life just don’t understand what I’m going through.” Just having other people who do understand the condition can really be an outlet for some of the frustration of dealing with these serious illnesses.
Striking a balance between selling and using data while protecting patients
Obviously, we’re on the forefront of this field, so finding a balance is very tricky and we work hard to maintain it. We let patients know, as best we can, the risks of sharing information so they can decide what they do or don’t want to share. In keeping with our philosophy, the patient is ultimately in control of how much they share.
In our partnerships, we explicitly say this data cannot be re-identified. They cannot use our website or other data sets to re-identify our patients. That way they’re just using the data to improve their business, and they are contractually obligated to not do some of the things they could do quite easily if they re-identified the data and attached it to individual patients.
Expanding the community
Our goal, long term, is to open Patients Like Me up to as many diseases as possible; currently, we have 19 conditions and 80,000 patients. While that’s a good start, we really want to open this community up to a wider audience. Our goal is a million patients in the next couple of years and give every last one of those patients tools to better manage and understand their illness.
Give us the freedom to innovate
BRUNO HOLTHOF, EX-MCKINSEY CONSULTANT AND CURRENTLY CEO OF ZNA, BELGIUM’S LARGEST HOSPITAL NETWORK, TALKS ABOUT THE FUTURE OF THE BELGIAN HEALTH CARE SYSTEM AND THE OBSTACLES TO OVERCOME.
Bruno Holthof is well-placed to have an opinion about the future of the Belgian health care. A medical doctor by training, Dr Holthof spent 15 years at consulting firm McKinsey&Company giving strategic advice to hospitals and pharmaceutical companies around the world. Since 2004 he is back in Belgium running the country’s largest hospital network. Comprising 3 general hospitals and 6 specialized hospitals, ZNA is also a top ten European health care provider. In this interview, Bruno offers his vision on the future of health care from a Belgian perspective.
Changing demographics and disease patterns
Let’s start by talking about the coming changes in the demand for health care, because that will have a dramatic impact on the way we need to organize our health care system. The main trend in this regard is the changing demography and the associated changes in disease patterns. We keep talking about the ‘graying’ of the population but in fact today we’re experiencing the ‘whitening’ of the population. What I mean is that we see a tremendous growth in the age categories 75+ and 85+. These people tend to have multiple organ malfunctioning. This means that we’ll need to treat these patients using a multidisciplinary approach and expand our geriatrics divisions. Furthermore, we will see a significant increase in dementia and hence we will need to increase our capacity for managing this condition, not only in institutional settings but also via home care and day care centers. All this is going to happen—we can predict this with confidence—and Antwerp will be hit fastest in Flanders.
Another key trend is the increasing birth rate, especially among immigrant families. This has implications for our pediatrics and maternity divisions. We also expect a further reduction in the maternity stay—from 4-5 days to 2- 3 days. Once we get to 3 days we’ll need to organize the entire process differently, probably by shifting to a single room model as opposed to moving the patient from a delivery room to a residential room.
Organizing around the needs of the patient
The advances in technology and medicine are making it possible to reduce stays for a whole range of conditions. Hence the hotel capacity of hospitals will need to be reduced and day care expanded. Such evolutions require a constant change in infrastructure, technology and organization. Children for example, are increasingly treated in day clinics. To better organize ourselves around the needs of the child we have been expanding our pediatric day clinic. The basic idea is to make sure that the flow through the day clinic is child friendly all the way and happens as smoothly and quickly as possible. At our hospital we’ve organized it as an adventurous journey from Green land to Sun land. The journey starts in Green land, a play area, where the child and the parents are welcomed and registered. The first diagnostic tests are done there. Then they move one to the next ‘country’ where they get their operating clothes and place their baggage in a locker. Afterwards it continues on foot or in a bed to the operating theatre. At the end of the journey the child arrives in Sun land where it is rewarded with an ice cream. At every stage we’re using playful methods to explain what is going on and the child can make choices too at several points in the process. It is a nice example of care being organized around the needs of the child and the parents.
Patients certainly are becoming more vocal and we need to adapt to this evolution. Also with regard to dementia for example, we are developing clear charters to make sure that we treat patients and their families with respect. It is important that we do not only focus on the medical side but also on, for example patient’s hair care and manicure because people with dementia tend to lose the ability to take care of themselves. It all has to do with respect.
Customized care
Customizing treatment to an individual’s needs and characteristics will also become increasingly important. Medicine has become much more complex and specialized; and it is constantly evolving and becoming more technology-intensive. In oncology, for example, we know that the effectiveness of certain types of chemotherapy is related to an individual patient’s genetic profile. As a result, therapy needs to be customized to the needs of the individual. Also in radiation therapy it is possible to do much more targeted and precise work, using sophisticated—and very expensive—equipment. In the coming years this trend toward more personalized care will only continue, not only on the basis of medical indicators but also on the basis of patient choice. It is true that many patients are becoming more vocal but in many cases they really have to be. For an increasing number of conditions—for example, prostate cancer, hip replacements, obesity, etc—there are several ways to treat it, hence it is essential that the patient is involved in the decision making.
Quality and the measurement of outcomes
The measurement of health care outcomes is becoming hugely important. At ZNA we’re making investments with the specific intent to start measuring outcome indicators. In 2011 we begin systematically measuring outcomes. Obviously you need to be very careful in the way you do this, especially in the way you correct for risk profiles. For example, an excellent maternity department could score really poorly if you just compared perinatal mortality rates in absolute terms. That’s because a reputable department will likely attract the most difficult cases.
Information Technology is enabling a more decentralized but connected health care system
Our ambition is to become a paperless hospital. We’re far from there, but we are investing with that intent. We will be setup with different form factors: mobile laptops, tablet PCs, smart phones, screens in rooms and operating theatres, etc. All our hospitals are already linked with a fiber network in preparation for the coming boom in data traffic. I expect a tremendous evolution in technology in the coming years. Imaging, for example, is becoming amazingly complex and this will certainly create a huge load on our network. For example, we recently streamed a live heart operation to a cardiology conference in Boston. These technologies enable much closer cooperation among different stakeholders and lines of care. For example, the multidisciplinary consult in oncology today requires people to come together physically. We’re currently exploring an advanced communication platform that will allow the caregivers to come together via video conferencing while they have access to all data and images from a common interface.
The key implication of all this technology is that we’ll need fewer large hospitals. In Flanders there was a trend to build large hospitals of 1000+ beds in a single location. In the future that won’t be necessary anymore. A degree of concentration is obviously still necessary to manage expensive medical equipment—patients need to come to the specialized infrastructure. But at the level of expertise you don’t need that concentration anymore. In the coming years a specialist will be able to deploy his or her expertise much more widely, even beyond borders. This is why I’m a proponent of smaller hospitals that are designed around the needs of the patients. Patients prefer smaller hospitals too. The future of health care will be more technological, more dispersed and more collaborative across the different lines of care. Our investment program is based on that vision.
An obsolete financing system is an obstacle to innovation
Innovation is critically important if we are to keep improving the quality and outcomes of health care—and keeping it affordable. The main obstacle to innovation, however, is our financing system. Our financing system is based on the retrospective payment of medical interventions and the duration of hospital stays. To illustrate, today in 2011 we still don’t know how much we will be paid for a hip replacement performed in 2006. Not only does that make financial planning very difficult but this type of system also often is a disincentive for investing in new technology and methods. Take obesity as an example. We know that we can’t just focus on surgery; equally important are psychological support and dieting to help patients reduce weight. But we don’t get financed for all that extra care. This is absurd. The financing should be linked to weight reduction outcomes; not just surgical intervention. As a hospital we should be funded on the basis of results, which would be a tremendous incentive to innovate, to invest in new technologies and methods.
Unfortunately there is lethargy in the system. You will always have stakeholders who resist change. That’s why I suspect that change will also have to come from patients. Patients are beginning to organize themselves via social networks – that’s a good thing. For example, we are seeing patients beginning to put political pressure on the way palliative care is funded. At present the government will only refund residential palliative care which has led to the closing of several day-care palliative initiatives – the only ones that survive are run by volunteers. But lobbying by patient groups should make an impact.
We Care
RUDY MATTHEUS, CHAIRMAN OF THE VOKA HEALTH COMMUNITY, OFFERS HIS VIEW ON THE CHALLENGES FACING BELGIAN HEALTHCARE AND THE POTENTIAL SOLUTIONS
As the European population ages and the prevalence of chronic disease rises, it is becoming increasingly clear that we can’t deliver higher-quality, more affordable healthcare without aligning payment incentives and improving coordination across the many providers who care for a given patient. New capabilities and healthcare models are required, which results in challenges and opportunities for our medical community, as well as our patient-clients.
The impact of the ageing population
New projections for 2010–2060, published by the European Office for Statistics, state that the number of elderly persons will rapidly increase, with the 80+ population group doubling in size by 2050. From 2015 on, deaths are projected to outnumber births in the EU27 and almost three times as many people will be 80 years or older in 2060. In Belgium (population 10 million) there are more than 1,8 million people older than 65 and 0,5 million people over 80. Eighty percent of people over 65 have a chronic disease and in the 75+ age group 85% has more than three chronic diseases.
These demographics trends will also be accompanied by a rapid growth in the number of persons with physical disabilities – about 21% of the 50+ population has severe vision/hearing/dexterity problems. Diabetes is now talked of as the epidemic of the 21st century, and parallels the worldwide explosion of heart disease.
The ageing of the European population and the associated rise in chronic conditions will lead to a growing number of older people living alone and in need of care. Simultaneously there will be astonishing but expensive advances in diagnosing and treating diseases, in a very personalized manner.
In light of these trends it is clear that the problem of care and assistance will become increasingly important both from a social and an economic perspective.
Healthcare models need to change
These trends pose a double challenge to existing healthcare delivery models. Firstly, there is a growing mismatch between traditional services and new needs – health services for example were originally designed to deal with acute rather than chronic disease. Secondly, rising demand for healthcare services is placing tremendous pressure on healthcare budgets. In response, the healthcare model will need to change dramatically. According to the Institute for Healthcare Improvement, “many healthcare systems around the world will become unsustainable by 2015. The only way to avoid this critical situation is to implement radical changes”.
New economic opportunities
The required changes will also create new economic opportunities. There are 85 million consumers in Europe over 65 years old today and this is expected to grow to 150 Million by 2050. Their combined wealth and revenues are estimated to be over €3000 billion. Clearly there is a tremendous opportunity to help empower elderly people to stay active and live independently. There also will be significant opportunities in the use of innovative approaches to improve care and make it more efficient. For example, the telecare market is expected to exceed €5 billion by 2015 in Europe alone.
Healthcare is already expanding in scope
Some significant changes are already in progress. Healthcare – traditionally focused on institutional care and on curing diseases (diagnosis, treatment) – is expanding in scope in at least two ways. The site of care is expanding its boundaries by going outside the hospital and the clinical setting and moving towards the patient’s home. And care is enlarging its scope beyond the patient domains to also encompass the support of people with special needs such as the elderly and the disabled.
Beyond the institution
Healthcare is extending its “institutional” role and is becoming personal, ubiquitous and mobile. Informal caregivers (patient’s family, friends, volunteers) are complementing the tasks of the medical professionals, but they are also under increasing pressure and need more tools. All citizens are becoming users of these new healthcare services and will be motivated and empowered to manage their own health. Currently we are witnessing a new wave of change: healthcare is pursuing a prevention objective, by focusing on health conditions through fitness, weight management and a generally healthier lifestyle. The social behavior and lifestyles, as well as the identity of the individual elder person, will change. Their requirements and consumer behavior will change both in quantitative and qualitative terms. A patient-client will become a consumer.
New capabilities required: care coordination and outcomes measurement
The new care delivery models demand capabilities for care service coordination and an ability to track quality outcomes that were not previously required in healthcare. This should apply to all services, also home-based services. Accreditation of services needs to be approached in a much broader way and should be stakeholder driven. The financial model needs to be reorganized; financial flows should be reallocated and become more outcome-driven. What matters are healthcare results and comfort levels; not the volume of medical interventions. The government should also investigate and rethink their financing role in building infrastructure where cost calculation should be based on life cycle costing and alternative financing should be explored. To support the move to team-based models of care, healthcare systems must accommodate the information and workflow requirements of the many stakeholders and organizations involved directly or indirectly in patient care. Social dimensions should also be taken into account. The coordination of information between all actors involved is crucial. In coordinated care the healthcare delivery system provides a continuum of evidence-based, quality driven healthcare services in a cost effective manner. Coordinated care requires a change in care culture, education, infrastructure, and in the relationships between patients, clinical staff, and caregivers. It calls for the creation of “accountable care cultures” that work together in coordinated, collaborative ways to drive better disease prevention, personalized treatment and positive outcomes. Technology can support this transformation by delivering vital information and tools that meet clinician and patient needs. Healthcare will address new user groups other than the traditional patients: the elderly and people with special needs such as persons with disabilities. By taking into account the ageing of the population, this new and additional “assisting” role of healthcare will become increasingly important. Ambient Assisted Living refers to intelligent systems of assistance for a better, healthier and safer life in the preferred living environment and covers concepts, products and services that interlink and improve new technologies and the social environment. It aims at enhancing the quality of life (the physical, mental and social well-being) for everyone (with a focus on elderly persons) in all stages of their life.
Quality of Life will have a new, extended meaning where physical, psychological and social aspects are taken into account all together and the “way the patient perceives his/her overall health status” will become of paramount importance. Perception will be more dominant in the evaluation and acceptance of the services.
Hospitals – which play a significant role in the health system – should increasingly try to differentiate and complement their offerings. One-day interventions will increase and care hotels will be the place where patient recover and rehabilitate before going home. We need to design for users; the solutions need to be user- and demand-driven. Care initiatives should:
- Respect patients’ values, preferences and expressed needs
- Coordinate and integrate care across boundaries of the system
- Provide the validated information, communication, and education that people need and want
- Guarantee physical comfort, emotional support, and the involvement of family and friends; the social component.
The user-as-producer transforms the relations between consumers and markets and among citizens themselves. Furthermore, it is opening up the possibility of reconfiguring the production process around the user. In many sectors there is a gradual incorporation of users into the process of production. All the stakeholders (patients and their families, medical professionals, policy makers, health organisations, industry, institutions, insurance companies, the overall community) need to find a way to cooperate in a common effort to create solutions for a new economy and added value for the patient.
Healthcare is an ecosystem – not a factory
The efficiency and effectiveness of healthcare services are certainly becoming a major priority. More integration of information is needed, as well as integration of the logistical processes through the whole value chain and core trajectory. But we need to be careful in comparing healthcare management approaches with those used in industry. While some processes (e.g. some logistical processes) are reasonably universal and hence can be standardized, care processes don’t always lend themselves to such standardization. Care processes are very often unpredictable and unplanned. We could best describe the healthcare model as an eco system. The intelligence is in the total care-system itself. There is chemistry to the way care functions; it a complex, adaptive system—and many aspects of care are distinctly artisanal in character. All actors in the healthcare delivery process should take that paradigm into account. The opportunity for creating new solutions and the needed delivery models should be part of such an ecosystem, where catalyst intelligence binds the demand and delivery elements. Health technology assessment and multi-sector innovative approaches will be needed to bring value added care towards customers and to create new business opportunities. As such, it is in this context that the idea of “we care” gains multiple dimensions—we care for people with our brains, hands and heart. Unfortunately the implementation of new approaches in healthcare is hampered by various challenges and restraints; they deal with technological issues and lack of standardization but also – and in some case preponderantly – with political, legal, financing and cultural issues.
